Section 18:
Identifying Major Classification of Arrhythmias from EKG Tracing
Rhythms that originate in the SINUS node:
• Regular sinus rhythm
• Sinus bradycardia
• Sinus tachycardia
• Sinus arrhythmia
EKG findings common to sinus rhythms:
• P wave present
• P wave is upright and rounded
• P wave amplitude less than 2.5 mm
• P wave duration less than 110 milliseconds
• QRS complex usually narrow
Normal Sinus Rhythm:
Normal sinus rhythm is 60-100x bpm. and shows all the following characteristics.
Use these five steps to analyze heart rhythms:
1) Is it Regular
2) heart rate between 60 and 100 bpm.
3) P to QRS Ratio
4) QRS interval of less than 0.12 seconds.
5) P-R interval between 0.12 and 0.20 seconds.
Basic Arrhythmias:
The SA node is the heart’s primary pacemaker. Heart rhythm can be affected if the SA node is not functioning properly.
Arrhythmias originating from the SA node are easily detected.
The P wave should be the focal point when analyzing the EKG strip.
Too Fast, Too Slow:
Sinus Tachycardia: The heart rate is simply too fast.
All other characteristics are normal except for the heart rate greater than 100x minutes.
Signs and symptoms: abnormal strong of forceful heartbeat, difficulty breathing, chest pain, anxiety, and change in the BP.
Most of the time, sinus tachycardia is a normal response of the cardiovascular system meant to the heart rate.
Tachycardia is normal during exercise or could be present with medical condition such as hyperthyroidism.
Treatment: vary depending on the underlying cause, but they usually involve a combination of lifestyle change (reducing caffein intake, quitting smoking, reducing sodium from diet) and medications
Sinus bradycardia rhythm: The heart rate is slow, all other characteristics are normal except for a heart rate of less than 60 x min.
Sinus bradycardia is not necessarily abnormal. For some athletes, patient how have medical conditions such hypothyroidism, or older adults who live a basically sedentary lifestyle, this rate might be normal.
Signs and symptoms: syncope, dizziness, fatigue, shortness of breath, chest pain, confusion, or memory problems.
Treatment: pacemaker
Atrial Dysrhythmias:
Atrial fibrillation: (often called A-fib) is a very common dysrhythmia , especially in older patients.
Atrial fibrillation makes the isoelectric line of the EKG tracing wavy and irregular with no clear P waves.
The QRS complex looks normal and has a normal duration, but the R-R interval is irregular.
Signs and symptoms: palpitations, weakness, fatigue, dizziness, shortness of breath chest pain.
Cause: hypertension, heart attack, coronary artery disease, abnormal heart valves.
Supraventricular Tachycardia:
Supraventricular tachycardia or narrow complex tachycardia (SVT): In this situation, the impulse is not following the normal electrical conduction pathway.
Heart rate will be greater than 150/min, P waves are usually not visible.
Signs and symptoms: fluttering in your chest, palpitations, shortness of breath, dizziness, sweating, syncope.
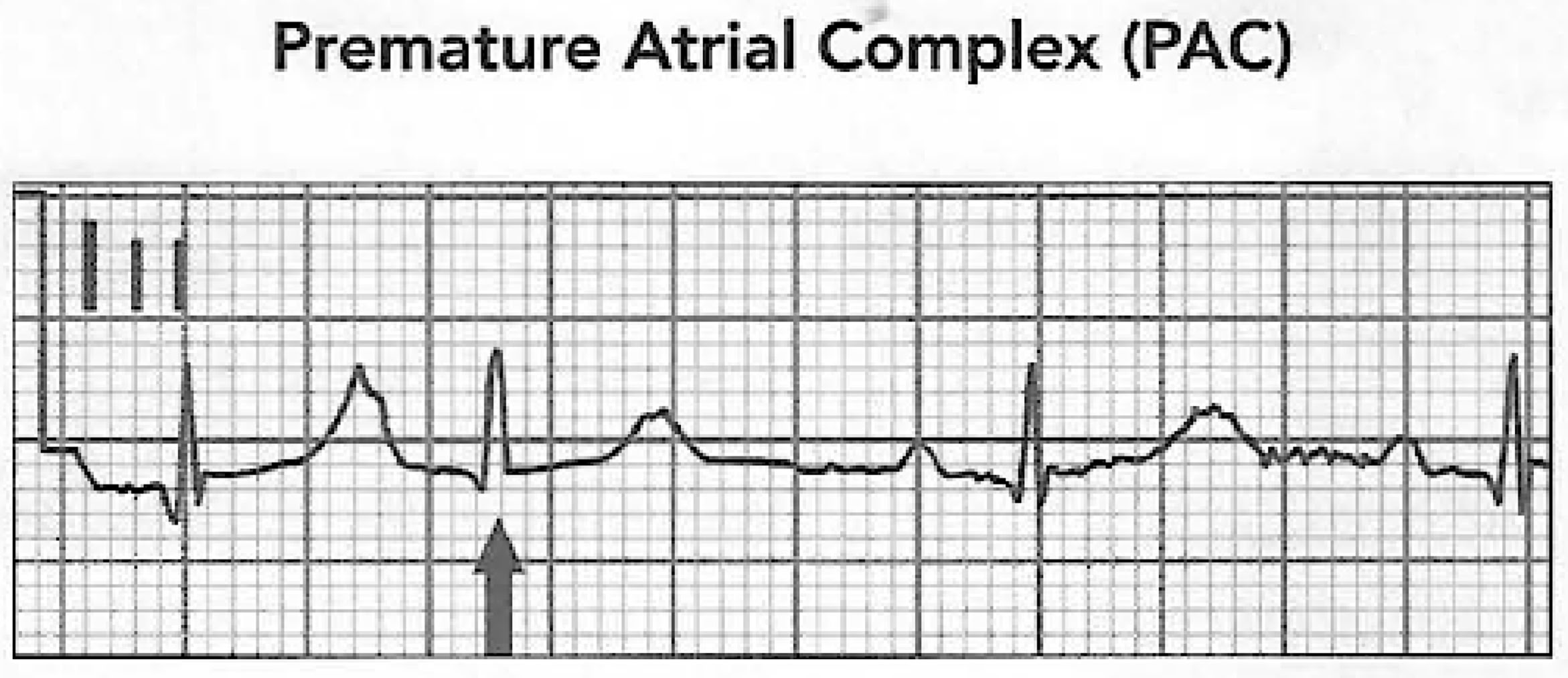
Premature Atrial Complex (PACs):
Premature atrial complex (PACS): are the result of electrical activity that originated in the atria.
The underlying rhythm is often normal but there are obvious early beats.
The QRS complex and the T wave in a premature atrial complex will be normal, but the P wave will not be normal, it may be buried in the preceding T wave, and the P-R interval may be shortened.
The P wave in these early beats may be taller and more pointed.
PACs are not rhythms! They are complexes that appear in an underlying rhythm.
First name the underlying rhythm, and then add PAC.
For example, the following tracing reveals regular sinus rhythm with one PAC.
The premature beat is the beat that occurs early in the cycle, followed by a rest period known as a compensatory pause.
This pause is a built-in delay mechanism enabling the heart to resume its electrical activity on time following a premature beat.
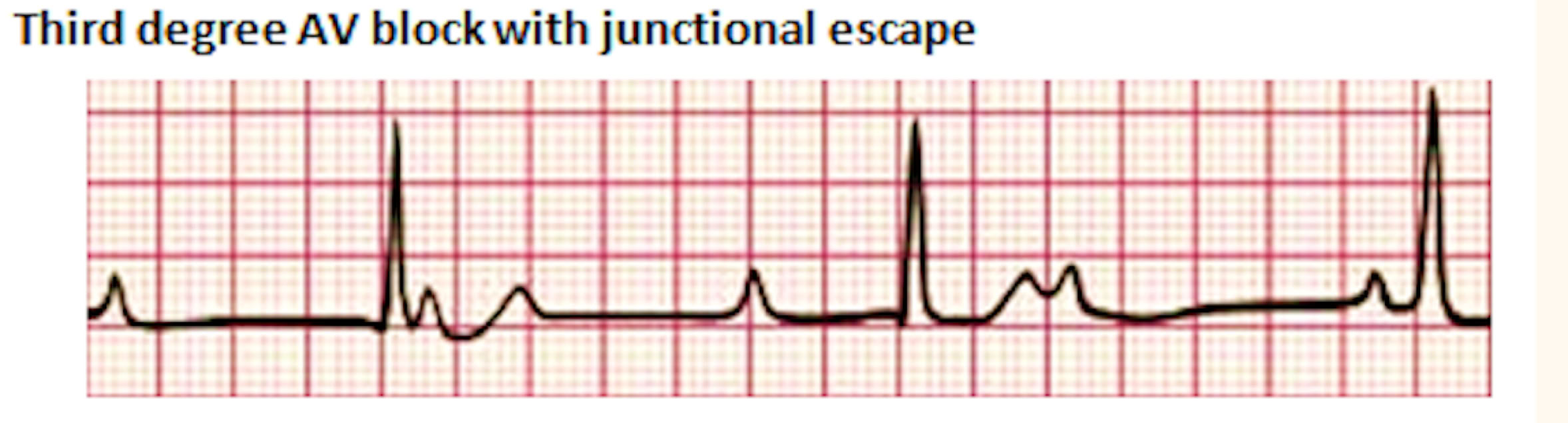
Heart Blocks:
Heart blocks are a special set of arrhythmias that indicate a difficulty in communication or no communication between the atria and ventricles.
In a normally functioning heart, the AV node and AV bundles slow down impulses from the SA node, allowing the ventricles time to fill with blood.
The severity depends on the location and cause of the blockage.
Heart blocks can usually be identified by a prolonged P-R interval.
First-degree heart block:
First-degree heart block represents a slow or delayed conduction through the AV node, resulting in a prolonged PR interval.
Specifically, the PR segment elongates in first-degree heart block.
P-R interval greater than 0.20sec
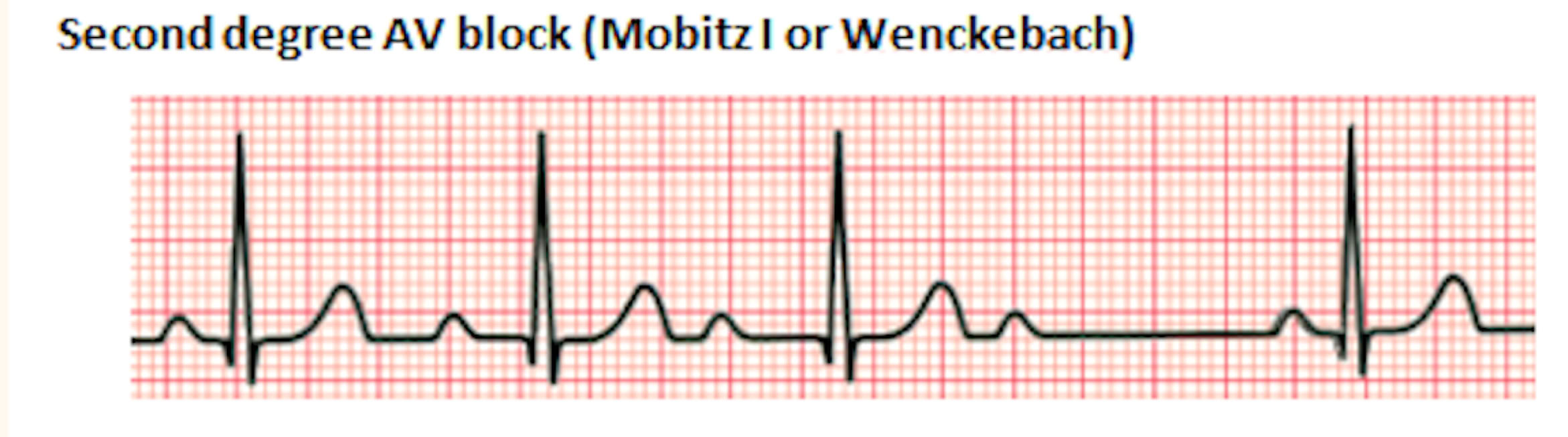
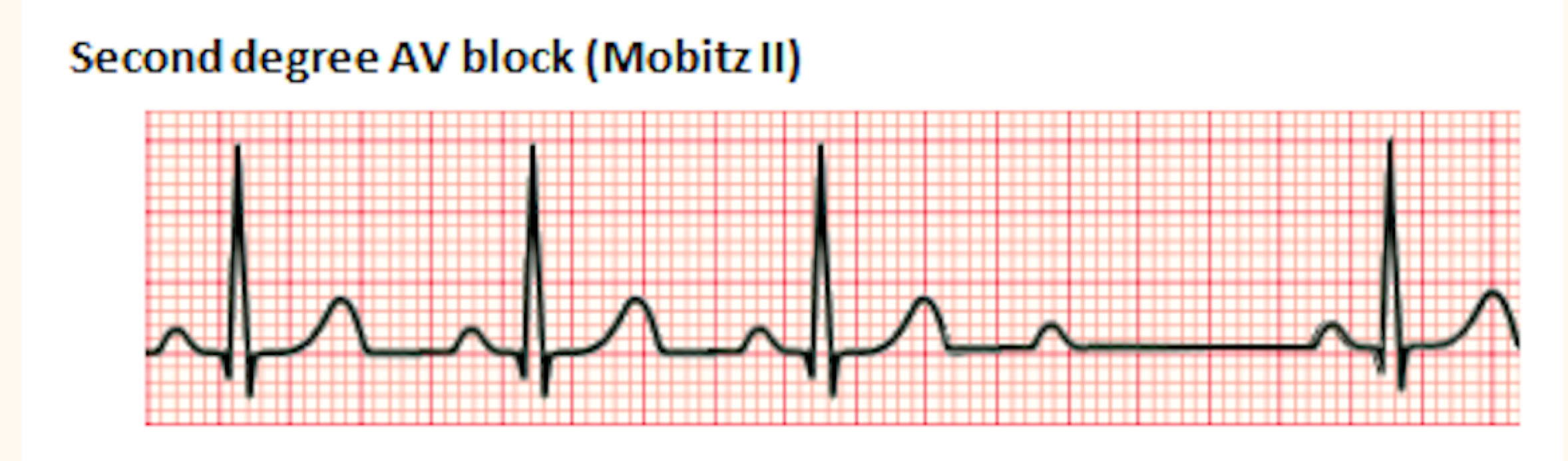
Second-degree Heart Block:
A second-degree heart block can occur in two forms:
Mobitz I (also sometimes called Wenckebach)
In this type of block, there are nonconductor or blocked impulses from the AV node to the ventricles.
As a result, there will be missing QRS complex. The P-R interval will get progressively longer until a QRS is missing, and then the patterns repeat itself.
Mobitz type II (second-degree atrioventricular block, type II)
This is the classic form of heart block. The P-R interval remains constant, but the P wave is present with no QRS complex or T wave.
In this situation, the AV node has selectively blocked specific impulses. This type of heart block tends to progress quickly to complete heart block.
Both types of Mobitz have some impulses that are totally blocked by the AV node, but the pattern of the block differs.
In the Mobitz type I the P-R interval of the conducted beats get longer and longer until a beat is totally blocked.
while in Mobitz ii the P-R segment is normal.
Heart Blocks Made Simple
Perform a normal arrhythmia interpretation on the tracing.
If you find more P waves than QRS complexes, evaluate the following:
1. Measure the RR interval
2. Measure the PR interval
If the RR interval is CONSTANT, the block must be second-degree type 2 or third-degree.
If the PR interval varies, how does it vary?
1. If it elongates, the block must be second-degree type 1.
2. If there is no association, the block must be third-degree.
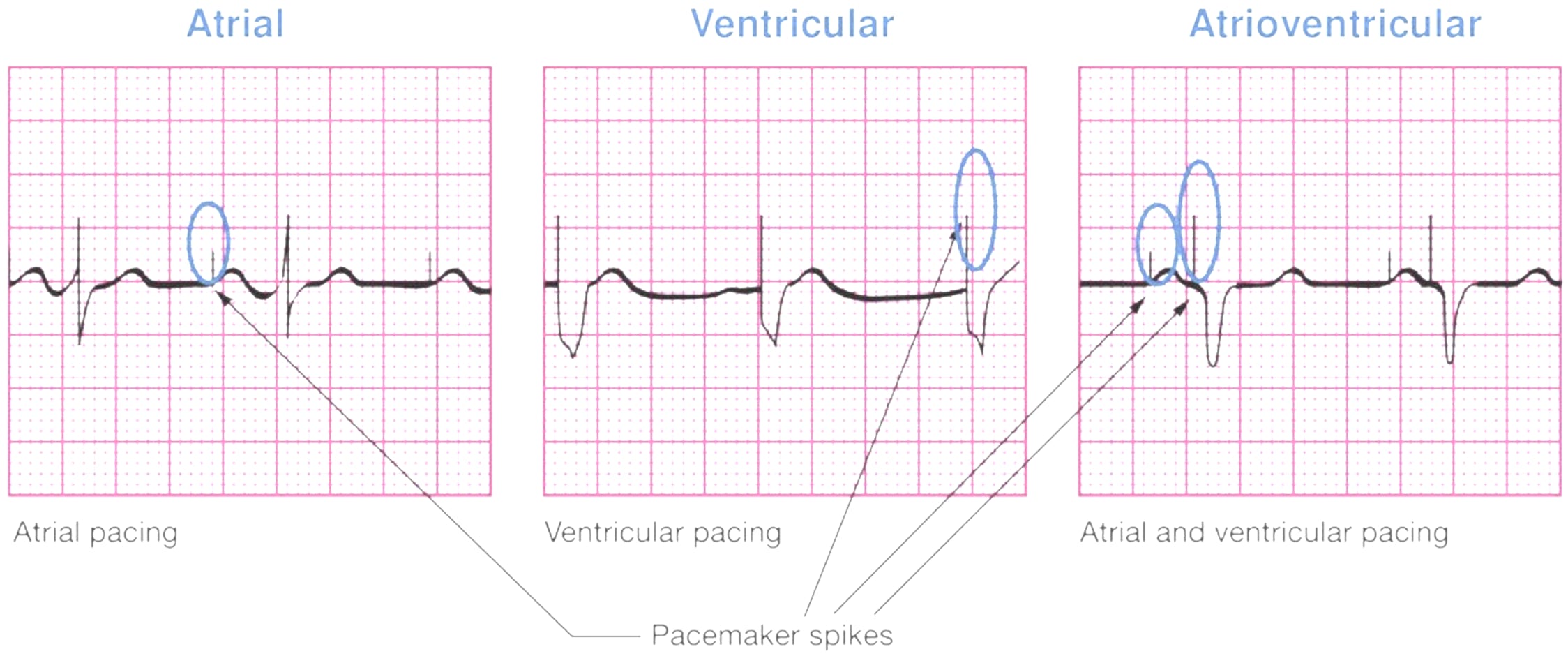
Pacemakers:
It is important to recognize artificially paced rhythms on a EKG tracing.
An artificial pacemaker is a device that is surgically implanted when a patient’s normal cardiac pacemaker no longer works properly.
Dysrhythmias (especially very slow rhythms) like Heart Blocks and Heart Failure are conditions that may require the placement of the pacemaker.
Pacemaker spikes: Pacing spikes are artifact in a EKG tracing that are a result of the electrical impulse produced by an artificial pacemaker.
They will appear as a thin spike at the P wave, QRS complex, or both, depending on the specific pacing needed and programmed.
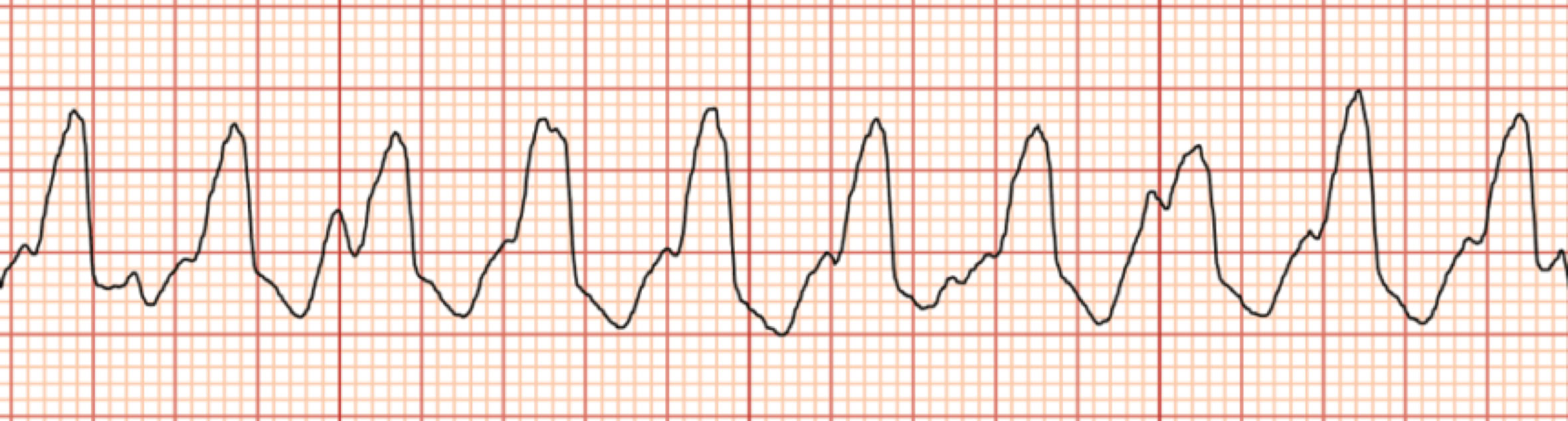
Ventricular Tachycardia:
Ventricular tachycardia (VT): is an extremely dangerous rhythm.
The rate is very fast, does not allow the coronary arteries or ventricles to fill, impairing cardiac output.
A patient may or may not have a palpable pulse when ventricular tachycardia starts.
There is a continuous state of contraction and relaxation of the ventricles, resulting in poor cardiac output.
There are no noticeable P waves in the tracing.
The QRS complex are wide and unusual, with a T wave deflected in the opposite direction.
Without intervention, it will progress quickly and decrease tissue oxygenation resulting in death.
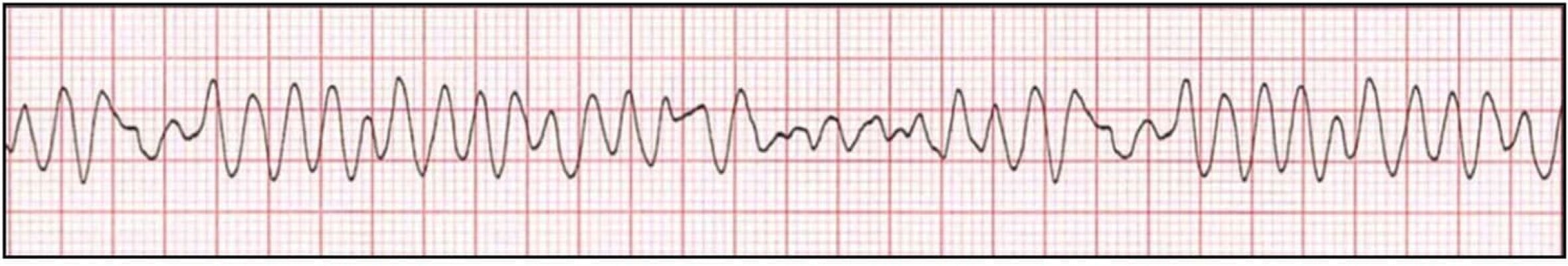
Ventricular Fibrillation:
Ventricular Fibrillation: is an emergency state in which the ventricles are not contracting and there is no cardiac output.
There are discernible waves noted throughout the tracing.
This dysrhythmia is not compatible with life.
Patients will likely be unconscious due to extremely poor cardiac output and tissue oxygenation.
Is considered a lethal dysrhythmia and requires immediate intervention to prevent death.
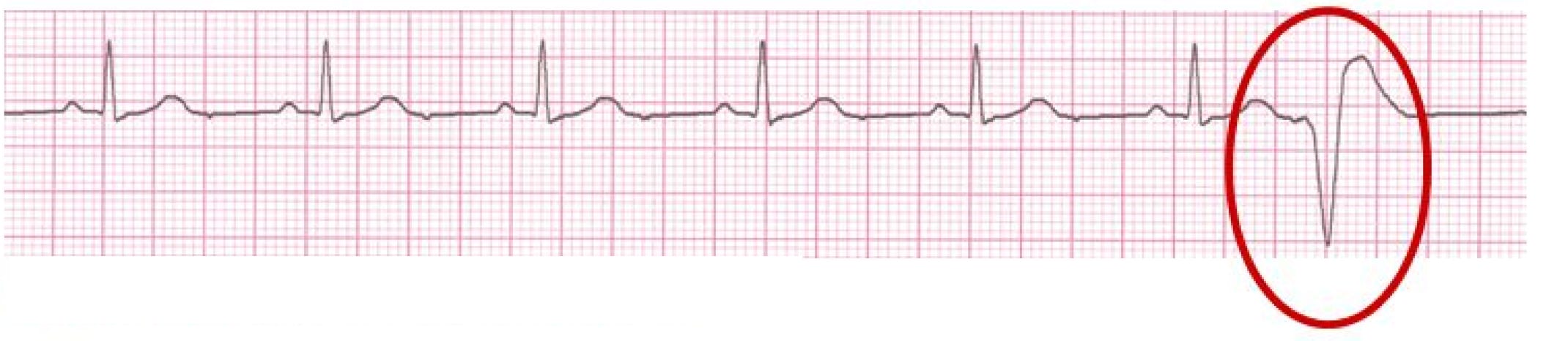
Premature Ventricular Complex (PVCs):
PVCs are ventricular depolarizations that occur early in the cardiac cycle. The characteristic findings on the EKG include:
• Absent P wave preceding the early QRS
• A wide QRS complex
• A QRS that looks different than the QRS complexes in the underlying rhythm
• The direction of the QRS complex and the T wave oppose one another
Like PACs, PVCs are not rhythms. They are complexes that appear in an underlying rhythm.
First name the underlying rhythm, then add PVC. For example, the tracing above reveals a regular sinus rhythm with PVCs.
PVCs can appear in many different patterns and with different shapes; in this case, the term "multifocal PVCs" is used which means the PVCs appear in groups.
Ventricular Escape Beats:
Ventricular escape beats: also, will have a widened bizarre QRS complex.
A ventricular rhythm with a rate of 20-40 bpm.
Idioventricular Rhythm:
Idioventricular rhythm: occurs when only the ventricular pacemaker is functioning.
When three or more ventricular escape beats occur in a row, it is considered an idioventricular rhythm.
The bpm is 20-40, and there are no discernible P waves.
The QRS complex is wide with an unusual appearance.
Agonal Rhythm:
Agonal rhythm: results when all the pacemakers of the heart (SA node, AV node, Purkinje fibers) have failed.
The tracing shows a wide, unusual QRS complex with no P or T wave.
The ventricular rate is less than 20/min.