Chapter 4: Dermal Puncture Equipment and Procedures
Dermal puncture or capstick is an alternative collection procedure when small amounts of blood are needed for testing, or for patients for whom venipuncture is inadvisable or impossible. It is the usual collection procedure for infants.
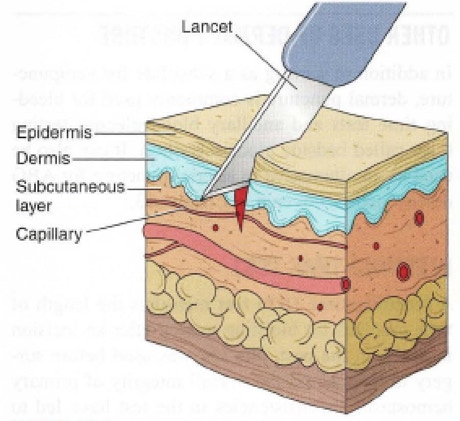
In addition, it is the standard procedure for blood glucose test. The depth of puncture must be carefully controlled to produce adequate flow while avoiding contact with underlying bone.
Dermal puncture is preferred in several situations and for several types of patients. Adult patients undergoing frequent glucose monitoring are excellent candidates for dermal puncture, because the test requires only a small amount of blood, which must be taken frequently.
Dermal puncture is usually the preferred method of collection for newborns, infants, and children younger than 2 years. Young children's smaller veins and lower blood volume make venipuncture both difficult and potentially dangerous.
Reducing blood volume through venipuncture is a concern for newborns and infants. It may lead to anemia and even cardiac arrest and death. However, some tests cannot be performed on blood from a dermal puncture. These include blood cultures and most routine coagulation tests.
DIFFERENCES BETWEEN VENOUS AND CAPILLARY BLOOD:
A dermal puncture collects blood from capillaries. Because capillaries are the bridges between arteries and veins, blood collected by , dermal puncture is a mixture of venous blood and arterial blood.
Small amounts of tissue fluid from the puncture site may be in the sample, especially in the first drop. Therefore the first drop which is also known as “Shock blood” must be wiped away and never used for testing.
EQUIPMENT FOR DERMAL PUNCTURE
Dermal puncture equipment allows the phlebotomist to puncture the skin safely and collect the sample quickly and efficiently, with a minimum of discomfort for the patient.
SKIN PUNCTURE DEVICES:
There are many types of skin puncture devices. The oldest and simplest is a handheld lancet, a thin, flat piece of steel with a very sharp tip. These are no
longer used due to Occupational Safety and Health Administration (OSHA) safety regulations that require a retractable blade on the puncture device;
instead, automatic devices have replaced these simple lancets in the modem health care environment.
Automatic puncture devices deliver a swift puncture to a predetermined depth, which can be a significant advantage at sites where the bone is close
to the skin.
The dimensions of the puncture are controlled by the width and depth of the point. Safety features include retractable blades and locks that keep a blade from being used a second time and prevent accidental sticks to the phlebotomist.

MICROSAMPLE CONTAINERS:
Containers come in different sizes to accommodate different volumes of blood. Micro-collection tubes and capillary tubes are made of plastic and are available with a variety of anticoagulants and additives.
The tubes are color coded by additive to match the coding of evacuated containers. Micro-collection tubes are used for all types of dermal puncture collections and are the most common type of collection containers used for dermal puncture samples.

ADDITIONAL SUPPLIES:
As in venipuncture, alcohol pads are used to prepare the site, and gauze pads are used to help stop the bleeding. A sharps disposal container is needed for
the lancet.
Warming devices increase circulation. Simple towels or washcloths may be soaked in warm water and applied to the site. Heel warmers are often used when blood must be collected from infants.
Be sure that the site is completely dry before puncture, however, as residual water will cause hemolysis and dilution of the specimen.
SITE SELECTION
GENERAL CONSIDERATIONS:
Dermal puncture should be performed on warm, healthy skin that is free of scars, cuts, bruises, and rashes.
The site must be easily accessible and have good capillary flow near the skin surface, but there must be enough clearance above the underlying bone to prevent the lancet from accidentally contacting it.
Bone puncture can lead to osteochondritis, a painful inflammation of the bone or cartilage, or osteomyelitis, a potentially serious, sometimes fatal, bone infection.
You should also avoid skin that has been damaged or compromised in any way. Specific areas to avoid include skin that is callused, scarred, burned, infected, bruised, edematous, or bluish.
PUNCTURE DEPTH AND WIDTH:
To minimize the risk of inflammation and infection, the lancet should never penetrate more than 3.0mm. For a heel puncture, the maximum depth is 2.0 mm, because the calcaneus, or heel bone, can lie very close to the surface.
DERMAL PUNCTURE SITES FOR ADULTS AND OLDER CHILDREN:
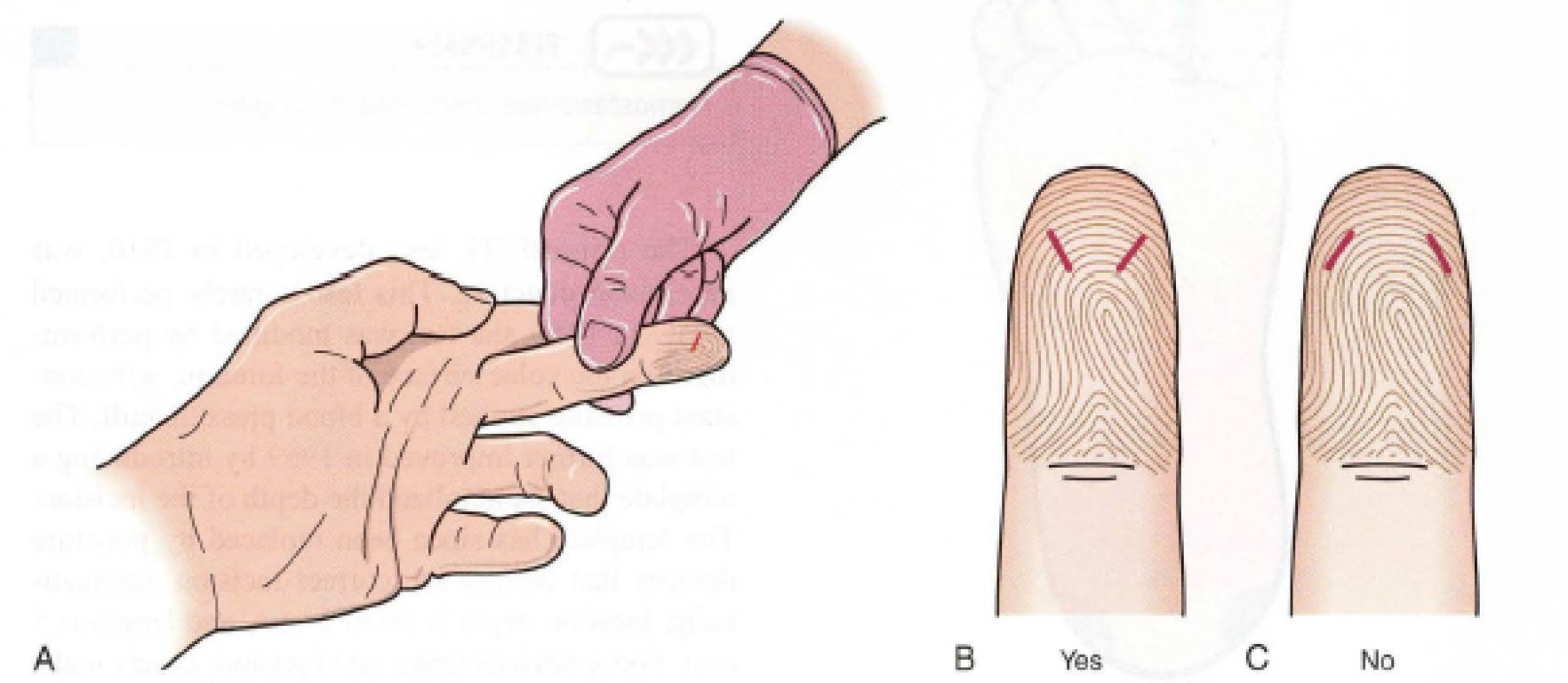
For adults and children older than 1 year, dermal punctures are almost always performed on the fingertips of the nondominant hand. The best sites are the palmar surface of the distal segments of the third (middle) and fourth (ring) fingers.
The thumb is likely to be callused, and the index finger's extra nerve endings make punctures more painful. The puncture should be made near the fleshy center of the chosen finger. Avoid the edge of the finger, as the underlying bone is too close to the surface.
The puncture should be made perpendicular to the ridges of the fingerprint, which lessens the flow of blood into the grooves.
DERMAL PUNCTURE SITES FOR INFANTS:
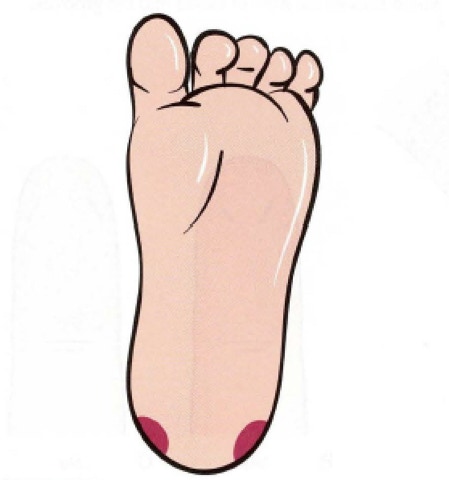
For children younger than I year, there is too little tissue available in any of the fingers. For this reason, dermal puncture is performed in the heel.
Only the medial and lateral borders of the plantar (bottom) surface can be used. The center of the plantar surface is too close to the calcaneus, as is the posterior (back) surface.
The arch is too close to nerves and tendons. For older infants, the big toe may be used if the heel is unacceptable. Be aware that the heel may be callused on young children who have started to walk.
Neonatal Screening:
Neonatal screening tests are used to detect inherited metabolic disorders that cause severe brain damage. This test is named Phenylketonuria Screening or PKU Test.
Specimen Collection:
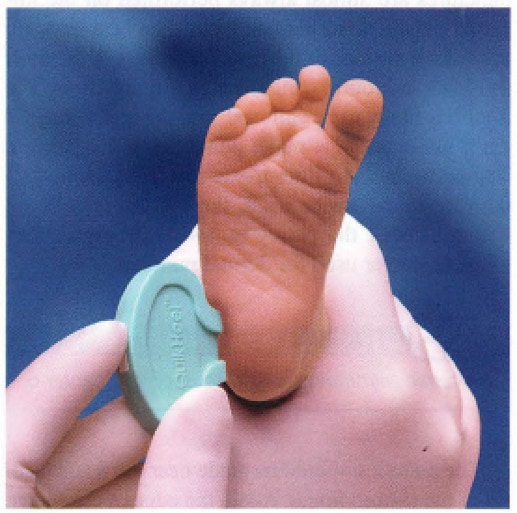
Blood for neonatal screening is collected by capillary heel stick on special filter paper.
The filter paper is supplied in a kit provided by the state agency responsible for screening tests.
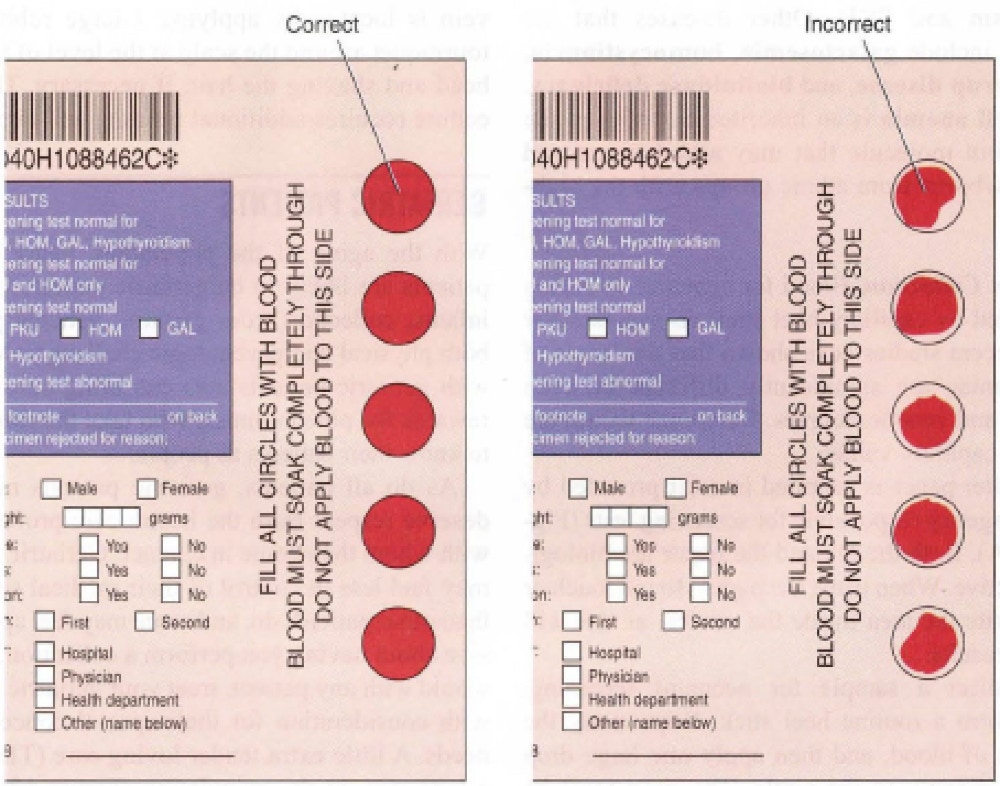
To collect this sample, first perform a routine heel stick. Wipe away the first drop of blood, and then apply one large drop of blood directly to the circle.
The drop must be evenly spread. Although applied to only one side of the filter paper, the blood should be visible from both sides.
Air-dry the specimen in a suspended horizontal position. Keep it at room temperature and away from direct sunlight until it is delivered to the lab.
Peripheral Blood Smear
Glass slides are used to prepare blood smears for microscopic examination of blood cells.
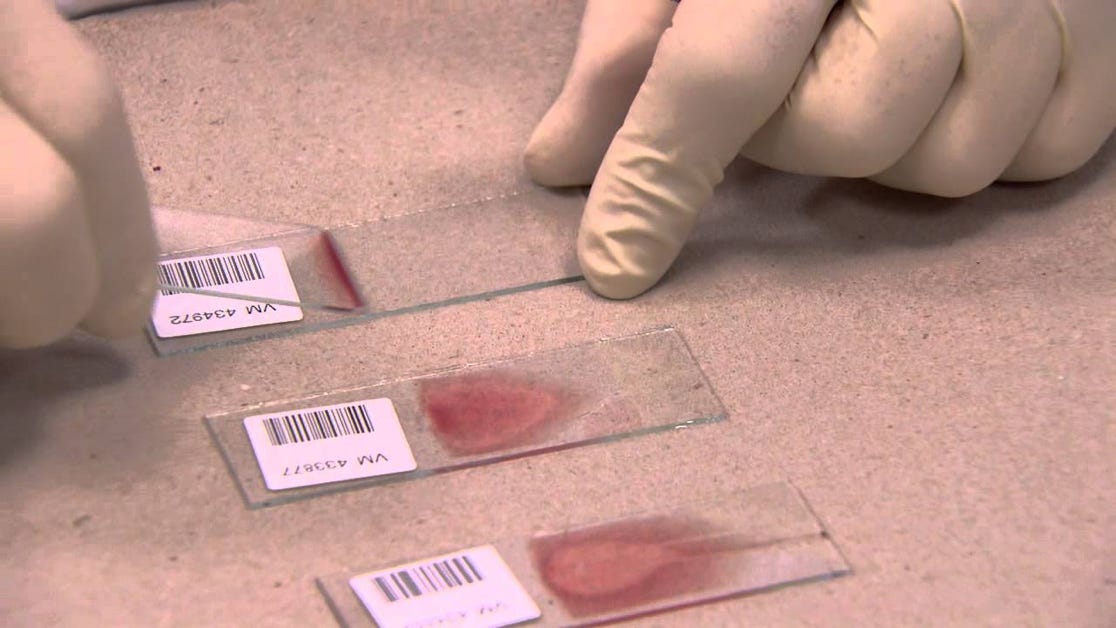
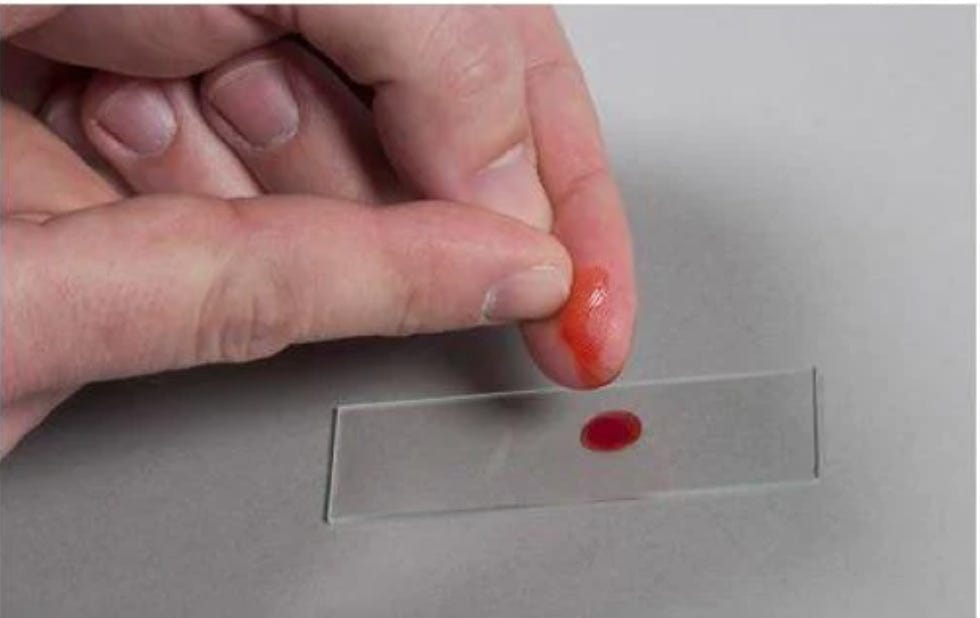
When performing a blood smear, the phlebotomist must assure that the blood forms feathered edges as shown in the picture above in order for the test to be conducted.
Capillary Puncture Procedure
.
