Although most venipuncture collections are routine and without problems, complications can arise. Many factors can interfere with the collection of blood, but most complications can be dealt with by knowing what to expect and planning ahead.
Complications include problems site selection, site cleaning, tourniquet application, sample collection, completion of the procedure, and sample integrity.
By learning the most common complications and the best approaches for avoiding or overcoming them, you will be better prepared in your work as a phlebotomist.
FACTORS THAT PREVENT ACCESS TO THE PATIENT
LOCATING THE PATIENT:
If the patient is not in the room, locate the patient by checking with the nursing station. If the patient is in another department and the test is a short turnaround time (stat) or timed request, proceed to that area and draw the blood there.
IDENTIFYING THE PATIENT:
Several situations can make lD difficult, including the following :
• Emergency room (ER) collections
• Orders telephoned in to the lab
• Mental incapacitation (Alzheimer’s Patient)
Despite the difficulties these situations may present, the information on the requisition must match exactly the information on the patient's ID band.
Any discrepancies must be resolved before collecting the specimen. When the ID band is missing, contact the nursing station so that one can be attached by the nurse on duty.
Even if an ID band is in the room, unless it is on the patient, you must not draw blood.
SLEEPING OR UNCONSCIOUS PATIENTS:
Never draw blood from a sleeping patient. Make one or two attempts to gently wake the patient.
If unsuccessful, you should contact the patient's nurse or your lab supervisor on how to proceed. The physician or nurse may give consent for you to proceed .
Unconscious patients are often encountered in the ER and intensive care unit (ICU). Treat an unconscious patient just as you would a conscious one, including identifying yourself and describing the procedure. Unconscious patients may be able to hear you, even if they cannot respond.
APPREHENSIVE PATIENTS:
Many patients have some apprehension about being stuck with a needle or having their blood drawn.
Most patients can be easily calmed by engaging them in a little distracting conversation on neutral topics, such as the weather, traffic, or news. If a patient is very nervous or you expect difficulty keeping the patient still or calm during the collection, it is helpful to request a nurse's assistance. This is especially true if the patient is a child.
PATIENT REFUSAL:
The patient always retains the right to refuse a blood collection. When a patient refuses to have his or her blood drawn, stress in a calm, professional way that the results are needed for treatment.
If the patient still refuses, document this on the request and notify the health care provider. Remember: never force a patient to have blood drawn.
PROBLEMS IN SITE SELECTION:
The antecubital fossa is the most common site for routine venipuncture. However, the presence of certain conditions at the chosen site may alter the quality of a specimen or cause harm to the patient. In that case, another site must be chosen.
OCCLUDED VEINS:
Veins that are occluded (blocked) or sclerosed (hardened) feel hard or cordlike and lack resiliency.
Occlusion can be caused by inflammation, disease, chemotherapy, or repeated venipunctures. Such veins are susceptible to infection, and because the blood flow is impaired, the sample may produce erroneous test results.
HEMATOMAS:
Hematomas may be caused by the needle going through the vein, by having the bevel opening only partially in the vein, or by failing to apply enough pressure after withdrawal. Blood from a hematoma is no longer fresh from the vein, and the hematoma can obstruct the vein, slowing blood flow. Each of these factors can alter test results.
EDEMATOUS TISSUE:
The arm may appear swollen due to the accumulation of tissue fluid or results when fluid from IV inflates surrounding tissues. Collection from edematous tissue alters tests results.
BURNS AND SCARS:
Areas with burns or scars are susceptible to infection and may be painful or difficult to penetrate.
MASTECTOMIES:
Mastectomy is the Surgical breast removal of breast tissue. A mastectomy causes lymphostasis, or lack of lymph fluid movement.
This can affect test results . The collection also may be painful to the patient, and the risk of infection may be increased. Your institution may require a physician 's consent before drawing on the same side as the mastectomy.
OTHER SITUATIONS
Any condition resulting in disruption of skin integrity means that the site should be avoided.
Open or weeping lesions, skin rashes, recent tattoos, or incompletely healed stitches are examples of sites that should be avoided because of the increased risk of infection.
DIFFICULTY FINDING A VEIN
When you cannot find a vein, several techniques can help.
Check the Other Arm
Examine the other arm for a suitable site. Ask the patient about sites of previous successful procedures.
Enhance Vein Prominence
• Dangle the arm in a downward position to increase blood in the arm.
• Rotate the wrist to increase the prominence of the cephalic vein.
• Tapping the antecubital area with the index and middle finger may help, but it increases the risk of damage to fragile skin and is not permitted.
Use a Blood Pressure Cuff
A blood pressure cuff can be used instead of a tourniquet or hard-to-find veins. Inflate the cuff halfway between the diastolic and the systolic readings. The phlebotomist needs special training to use the blood pressure cuff in this way.
Use an Alternative Site
When a suitable vein cannot be found in the antecubital fossa, you will have to collect the blood from somewhere else-the hand, foot, or leg. The leg and foot are more susceptible to infections and clots, and they are not recommended sites for patients with diabetes or those on anticoagulant therapy (heparin or warfarin). Collection from the leg and foot usually
requires the physician's permission.
PROBLEMS ASSOCIATED WITH CLEANING THE SITE
Alcohol cannot be used for site cleaning when drawing a blood alcohol test. The alcohol may raise the patients blood alcohol level and render an inaccurate reading.
PROBLEMS ASSOCIATED WITH TOURNIQUET APPLICATION
HEMOCONCENTRATION:
A tourniquet should not remain in place for more than 1 minute at a
time. This is to prevent hemoconcentration, or alteration in the ratio of elements in the blood.
These problems can be avoided by releasing the tourniquet as soon as blood flow begins in the first tube.
Hemoconcentration can also be caused by pumping of the fist
FORMATION OF PETECHIAE:
Petechiae are small, nonraised red spots that appear on the skin when the tourniquet is too tightly.
The appearance of petechiae indicates that the site may bleed excessively after the procedure and requires longer application of pressure on the puncture site.
TOURNIQUET APPLIED TOO TIGHTLY:
If there is no arterial pulse or the patient complains of pinching or numbing of the arm, the tourniquet is too tight. Loosen it slightly before proceeding.
LATEX ALLERGY:
Latex allergy is becoming increasingly common, and all patients must be asked whether they have a latex allergy. Nonlatex tourniquets and gloves are available. Latex bandages should also be avoided for these patients.
COMPLICATIONS DURING COLLECTION
CHANGES IN PATIENT STATUS:
In all of the following cases, be sure your patient is in a safe position before leaving the room.
Syncope:
Syncope is the medical term for fainting. The patient's skin often feels cold, damp, and clammy before syncope. If syncope occurs during the procedure, remove the tourniquet and needle immediately and apply pressure to the site.
If the patient is conscious but woozy, have the patient remain seated and in a safe position. Call a nurse to check the patient's blood pressure. If the patient is unconscious, call the nurse immediately.
The patient should be safely moved to a recumbent (lying down) position until he or she regains consciousness. All incidents of syncope must be documented.
Seizures:
If a patient has a seizure during the procedure, remove the tourniquet and needle immediately and apply pressure to the site . Do not put anything in the patient's mouth; this is of no use during a seizure and can cause injury.
Nausea and Vomiting (Emesis):
When emesis occurs, reassure the patient and make him or her comfortable. Give the patient an emesis basin, and instruct him or her to breathe slowly and deeply. A wet washcloth for the head is often helpful.
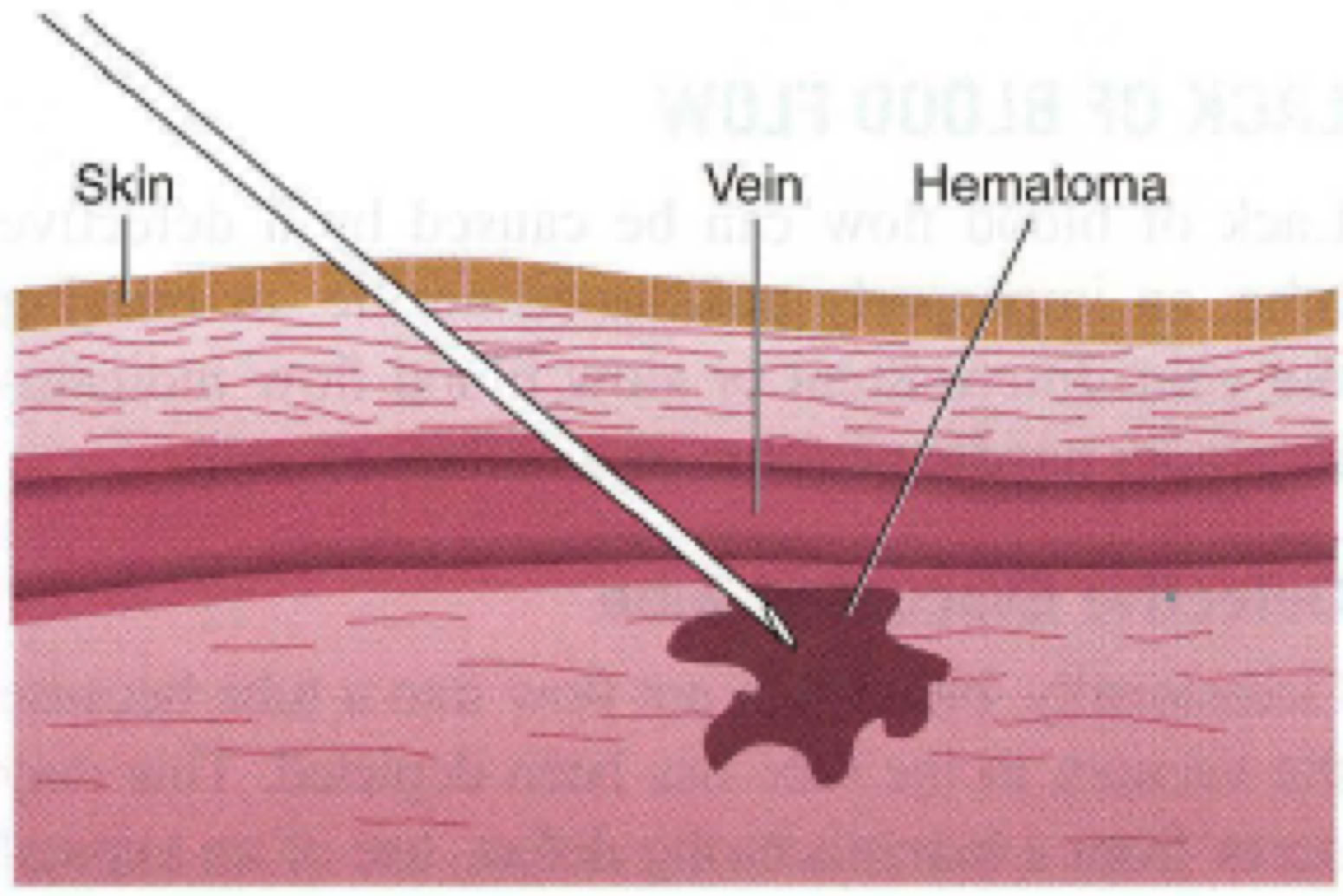
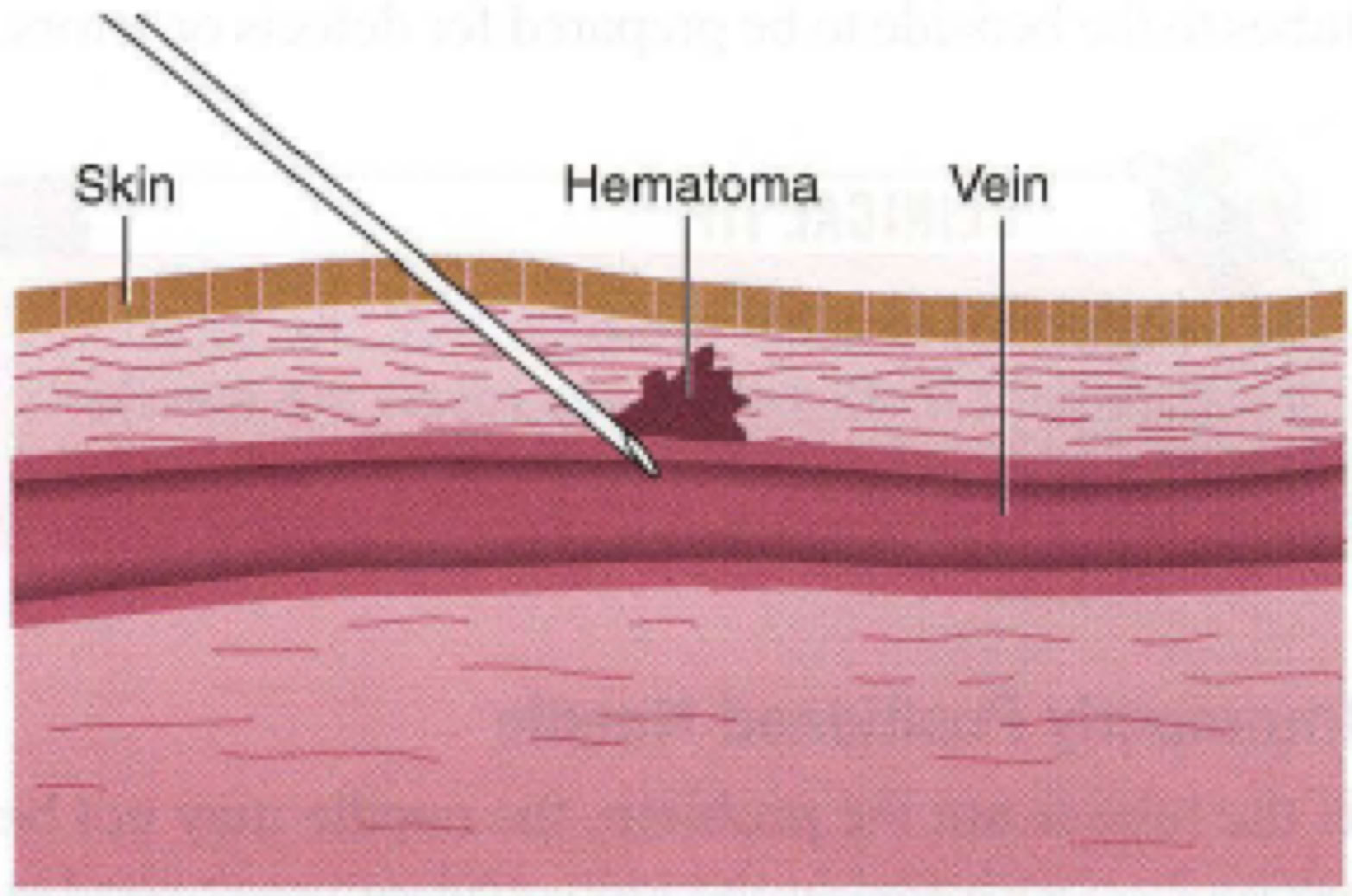
Hematoma:
When blood oozes from the vein into the surrounding tissue, a hematoma or bruise is formed. You can see the skin surrounding the puncture swell up and fill with blood.
If this occurs during the procedure, remove the tourniquet and needle immediately and apply pressure to the site. A cool cloth or cold pack can slow swelling from blood and ease pain.
The following are the most common causes of
hematoma are:
• Excessive probing to obtain blood
• Failure to insert the needle far enough into the vein
• The needle going through the vein
• Failure to remove the tourniquet before removing the needle
• Inadequate pressure on the site after removal of the needle
• Bending the elbow while applying pressure
LACK OF BLOOD FLOW
Lack of blood flow can be caused by a defective tube, an improperly positioned needle, or missing the vein. Intermittent or slow blood flow may indicate improper needle position or a collapsed vein.
Defective Evacuated Tube:
Occasionally, blood will not flow into a tube because the vacuum in the tube has been depleted. This may occur from a manufacturing defect, use of an expired tube, or a very fine crack (which may occur if the tube is dropped).
Always take extra tubes to the bedside to be prepared for defects or errors.
Improperly Positioned Needle:
If the tube is not the problem, the needle may not be properly positioned in the vein, and you may need to adjust it. When the needle is not in the correct position with respect to the vein, blood flow may stop or may be intermittent. Any one of the following may have occurred:
• The bevel is stuck to the vein wall. Slightly rotate the needle
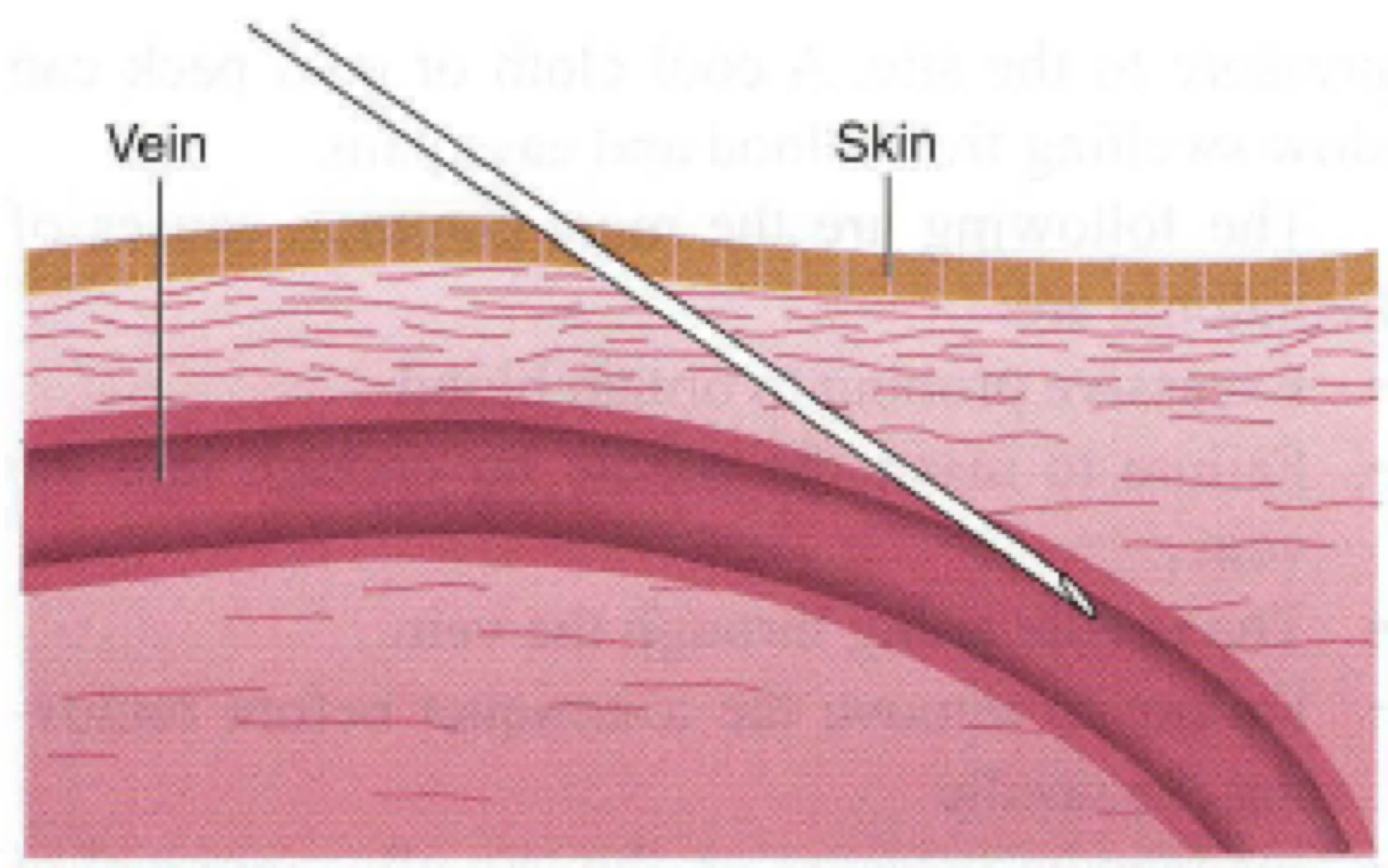
• The needle has passed through both sides of the vein ("blowing" the vein). Slowly pull back on the needle
• The needle is not advanced far enough into the vein. Slowly advance the needle.
• The vein was missed completely. Pull the needle out slightly, palpate to relocate the vein, and redirect the needle.
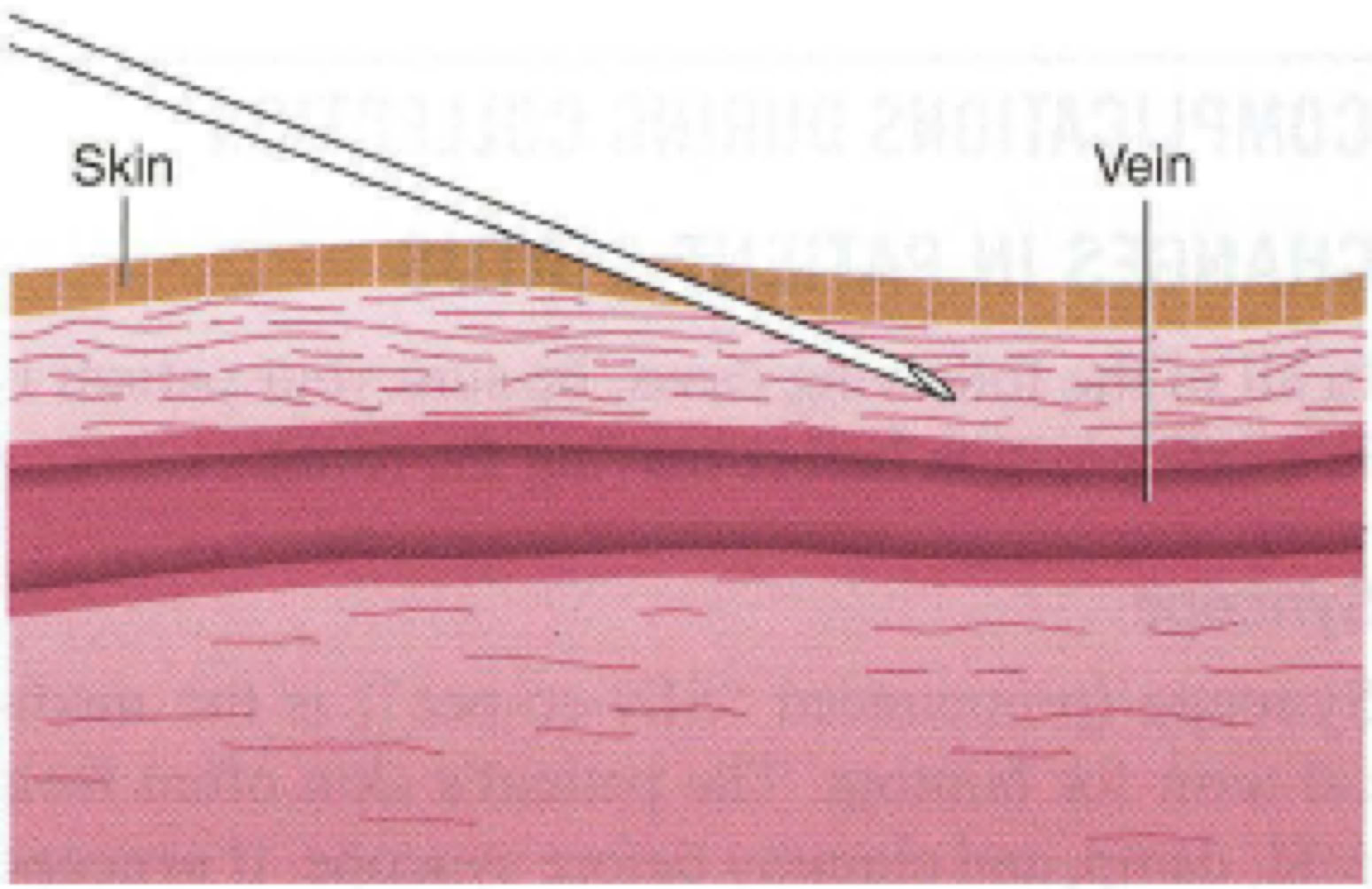
COLLAPSED VEIN:
A collapsed vein is caused by too much vacuum on a small vein. When using the evacuated tube system.
During a syringe collection, it may occur when the plunger is pulled too quickly. Using smaller tubes or pulling the syringe plunger more gently can help prevent collapsed veins. Once a vein collapses, remove the tourniquet, pull out the needle, and select a different vein.
INADVERTENT PUNCTURE OF THE ARTERY:
Puncture of the artery produces bright red blood and may cause spurting or pulsing of blood into the tube. Withdrawal needle and apply pressure for 10 minutes.
FAILURE TO COLLECT ON THE FIRST TRY:
The policy at most institutions is that a second try is acceptable. A new needle and tube must be used. For second tries, go below the previous site or use the other arm. After a second unsuccessful try, another phlebotomist should be found to draw blood from the patient.
PROBLEMS IN COMPLETING THE PROCEDURE
PATIENT REQUESTS:
Sometimes a patient may ask you for water or a change in bed position. Always check with the nurse on duty before you comply with any request.
PROLONGED BLEEDING:
Normally, the site should stop bleeding within 5 minutes. However, aspirin or anticoagulant therapy can prolong bleeding times after the venipuncture
procedure.
In all cases, you must continue to apply pressure until the bleeding has stopped. Inform the nurse if the patient has a prolonged bleeding time.
Failure to apply adequate pressure, particularly with patients on excessive doses of warfarin (Coumadin) or with a coagulation disorder, can cause compartment syndrome. In these patients, it is important to apply pressure to the site beyond 5 minutes and ask the patient about any symptoms or significant pain.
FACTORS THAT AFFECT SAMPLE INTEGRITY
HEMOLYSIS:
Hemolysis is the destruction of blood cells. Hemolysis can be caused by a range of factors. The serum or plasma is pinkish or red in a hemolyzed sample due to rupture of red blood cells. The lab may request a redraw if the sample cannot give accurate results for the requested test.
BLOOD DRAWN FROM A HEMATOMA:
The blood in a hematoma is older than fresh venous blood, and use of such a sample can alter the results of some tests.
REFLUX OF ANTICOAGULANT:
Reflux is the flow of blood from the collection tube back into the needle and then into the patient's vein. This is rare, but it can occur when the tube contents come in contact with the stopper during the draw.
Anticoagulant, as well as blood, may be drawn back into the patient's vein. This is a problem, because some patients have adverse reactions to anticoagulants and loss of additive from the tube can alter test results.
It may also result in the contamination of the next tube with additive from the previous tube. To prevent reflux, keep the patient's arm angled downward so that the tube is always below the site, allowing it to fill from the bottom up.
LONG-TERM COMPLICATIONS ASSOCIATED WITH VENIPUNCTURE
IATROGENIC ANEMIA:
Life is threatened if more than10% of blood volume is removed at once. For this reason, it is important to minimize the amount of blood drawn and the frequency of collection. Your institution should have a procedure in place for documenting the total volume of blood drawn from a patient.
COMPARTMENT SYNDROME:
For patients receiving excessive doses of anticoagulants such as warfarin, routine venipuncture may cause bleeding into the tissue surrounding the puncture site .
A small amount of blood leads to a hematoma, larger amounts may cause compartment syndrome, which is a condition in which pressure within the tissue prevents blood from flowing freely in the blood vessels.
This causes swelling and pain, and it carries the risk of permanent damage to nerves and other tissues . Severe pain, burning, and numbness may be followed by paralysis distal to the puncture site.
The patient should seek immediate medical attention if compartment syndrome is suspected.
NERVE DAMAGE:
Nerves in the antecubital area can be damaged if they are contacted with the needle during collection. The patient will experience a shooting pain or "electric shock" sensation down the arm, numbness, or tingling in the fingers.
If the patient experiences this type of sensation, immediately remove the needle. This incident should be documented according to your institution 's protocol. To prevent nerve damage, avoid excessive or blind probing during venipuncture.
INFECTION:
Infection can be prevented by proper aseptic technique before and during collection and by keeping the bandage on for at least 15 minutes afterward.
Outpatients should be instructed to leave the bandage in place for at least that long.
SPECIMEN REJECTION:
Specimens may be rejected by the lab for a variety of reasons:
Collection in the wrong tube
Contaminated specimens and containers
Hemolysis
Improper special handling
Incompletely or inadequately filled tube
Unlabeled or mislabeled specimens
Almost all of these can be avoided by proper care before, during, and after the procedure.
SPECIMEN RECOLLECTION:
Sometimes, problems with the sample cannot be identified until after testing. In this case, another sample will have to be collected
Pediatric Venipuncture
Challenges
-Small, undeveloped veins
-Considerable risk of permanent damage
-Smaller blood volume in body; risk for iatrogenic anemia
Dealing with Parents or Guardians
-Earn trust the by being warm, friendly calm, confident & caring
-Ask about child past expert
-Allow to stay in room, if desired
Dealing with the child
-Gain trust; approach slowly & determine level of anxiety
-Explain procedure in terms a child can understand
-Emphasize importance or remaining still
-Offer reward for cooperation
Pain Interventions
-Eutectic mixture of local anesthetics (EMLA)
-Available in a cream & in oral solution
-Takes about 1 hour to anesthetize area
Selecting a Method of Restraint
-Infants: Wrap in a blanket
-Toddlers: have parent hold on lap
Equipment Selection:
23 gauge butterfly needle attached to an evacuated tube or syringe
Collect minimum amount of blood required for testing
Geriatric Venipuncture
Challenges
-Skin changes
-Hearing impairment
-Visual impairment
-Mental impairment
Equipment Selection:
23 gauge butterfly needle attached to an evacuated tube or syringe
Tourniquet Application:
Loose enough to not damage skin
Site selection:
avoid bruised areas from previous venipuncture
Performing the Venipuncture:
anchor vein firmly to avoid rolling
Patients on Dialysis and Other Settings
Dialysis Patients
-Do not use arm with AV Fistula for venipuncture
