Module 4:
Communication and Patient Lifespan

As a Healthcare Worker, you will be a key communicator between the facility and patients.
You will be required to explain procedures, ask, and answer questions, and meeting patient needs will be part of your tasks.
Developing strong communication skills is the ability to effectively relay information to patients, family members and other medical professionals. This skill is needed in the medical office and is just as important as mastering administrative and clinical task.
Customer service is the friendly and courteous treatment of all persons entering the facility and is the most important part of communication to families and patients.
Prior to performing any tasks, inform the patient about the procedure to build trust an alleviate anxiety. The patient must understand the procedure to provide consent.
To facilitate communication, maintain a nonjudgmental attitude and demonstrate good listening skills.
Listening Skills are summarized as the ability to listen, understand and assure the message sender that you understand their message.
Communication Factors:
Message Sender:
the person who wants to communicate information
Message:
the information the person needs to send
Receiver:
person to whom the message is sent
Confirmation:
the way the receiver lets the sender know that the message has been received.
Types of communication
Verbal Communication:
spoken or written words

Non-verbal Communication:
facial expressions, posture, hand/body movements, and appearance

Written Communication:
Communication relayed in writing , examples are the patients care plan or patients electronic medical record

To have a good communication is important to:
Maintain eye contact whenever is possible.
Face the patient.
Repeat or clarify what the patient says.
Patients who have cognitive disabilities can require extra time to ensure
that they understand the procedure.
Cognitive Disabilities are mental impairments that affect the persons understanding and descision making abilities.
Additionally, people who have sensory impairments (vision impairment, hearing loss, dysphasia) can require additional audiovisual media, such as written materials, pictures, or audio files.

If the patient and the technician do not speak the same language, communicate through a trained Medical Interpreter. A medical Interpreter is a staff member who speaks the native language of the patient. All patients legally must have access to trained interpreter who speaks their native language. There for, all facilities have a medical interpreter department where you can request a person who speaks the patients native language for translation. Avoid using family members as interpreters; they may not communicate information accurately.
There may be obstacles when communicating with Patients, it is important that you consider these barriers of communication.
If your message was not heard correctly or not understood by the patient
If the resident cannot hear due to loss of hearing
you used words that the resident does not understand
You must always assure the patient clearly understands what you are communicating with them.
Sometimes when Residents cannot cope with stress, they may becomes defensive, these are some common defense mechanisms:
Denial (“I didn’t do that”)
Projection(Telling you that you did something that they did)
Displacement (They try to focus the attention on something someone else did)
Rationalization (They try to justify why they did something)
Repression (They try to insult or belittle you)
Regression (They go to a child like behavior, Pretend they can’t hear you, put their head down, act like a child)
When you are communicating with a patient, there is two types of information that will be received.
Objective Information
Information based on what you see, hear, touch or smell (based on your senses)
Subjective information
Information that cannot be or was not observed by you; it is based on what a patient thinks or something that was reported by a patient that may or may not be true
residents who have sensory losses
residents who have memory losses
residents who have vision loss
residents who have hearing loss
residents who have problems with speaking
residents who have problems with understanding
How can a NA assist residents with hearing impairment?

Make sure hearing aid is on and working
Reduce or remove distracting noise
Get resident’s attention before speaking
Speak clearly, slowly and in good lighting
Do not shout or mouth out words in an exaggerated way
Keep hands away from face while talking
THERAPEUTIC COMMUNICATION

Therapeutic Communication: the face-to-face process of interacting that focuses on advancing the physical and emotional well-being of a resident.
Therapeutic communication is the basis of interactive relationships and affords the healthcare worker the opportunity to establish rapport, understand the Patient’s experiences, formulate individualized interventions and optimize the care they provide to the Patient.
Active Listening: Being attentive to what the Patient is saying, verbally and non- verbally. Sit facing the Patient, open posture, lean toward the Patient, make eye contact, and relax.
Providing Information: Relevant information that is important to make decisions, experience less anxiety, and feel safe and secure.
Clarifying: To check whether understanding is accurate, or to better understand, the EKG Technician restates an unclear or ambiguous message to clarify the meaning. “I’m not sure I understand what you mean by ‘sicker than usual’, what is different now?”
Summarizing: Pulls together information for documentation. Gives the Patient a sense you understand. It is a concise review of key aspects of your interaction.
UNDERSTANDING HUMAN BEHAVIOR
Understanding human behavior is important when you are communicating with patients.A healthcare worker is exposed to many different personality types in addition to different illnesses.
When you understand why a person is behaving in a certain way, you can adjust your communication style to adapt to that person.
Abraham Maslow, a psychologist, studied the basic human needs that motivate people.
He identified 5 basic human needs and arranged them in a pyramid to show their order from the most basic to the highest level needs.

Maslow’s theory is that people strive to meet their unmet needs, but the most basic needs must be met before the person is free to meet the needs at the next higher level.
A Human Being has six basic needs:
Food and water
Protection and shelter
Activity
Sleep and rest
Safety
Comfort, freedom from pain
Psychosocial Needs
Are needs having to do with social interaction, emotions, intellect, & spirituality
A human being has the following psychosocial needs:
Love and affection
Acceptance by others
Security
Self-reliance and independence in daily living
Sexuality and Intimacy

People continue to have sexual needs through their lives
Humans express their sexuality through different behaviors
Knock and wait for a response before entering resident’s rooms
Provide privacy if you encounter a sexual situation.
Spiritual Needs

As an NA you can help your residents with spiritual needs:
Learn about their religion
Assist with practice (never make judgments)
Respect all religious items
Report requests to see clergy to nurse
You should never:
Try to change someone’s religion
Tell a resident his/her belief or religion is wrong
Express judgments about a religious group
Holistic Care:
a type of care that involves considering a whole system, such as a whole person.
Cultural Diversity

Cultural Diversity:
people with varied backgrounds, experience and culture who live and work together in the world
Culture plays a part in determining all of these things:
Language
religion
food preferences
degree of comfort with touch
Patients and their Families

Families play an important role in the care of residents, they are vital in these and other ways:
Making Care Decisions
Communicating with the care team
Providing support and encouragement
Connecting with the Outside world
NA’s must treat residents’ families and friends in a professional manner, be respectful and nice
allow privacy for visits
Observe and report effects of visits on residents.
Remember Protected Health Information should never be shared with family or friends.
Lifespan and Development
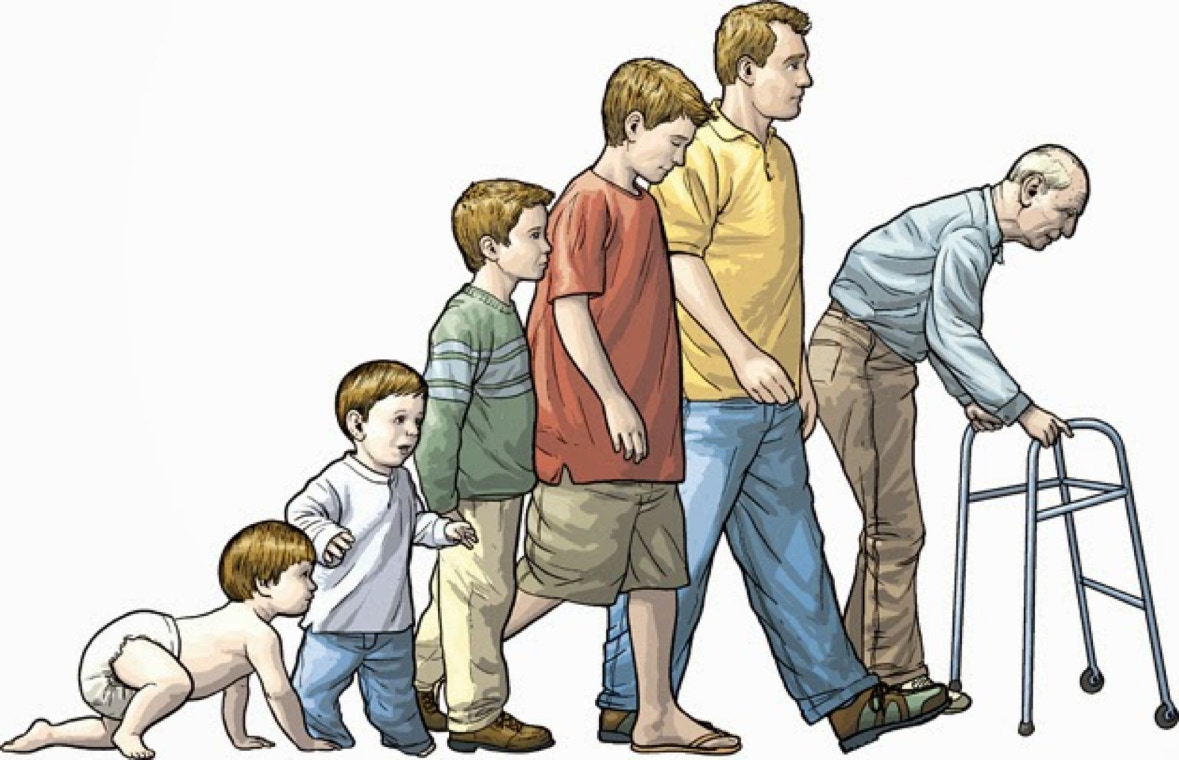
Patients go through many changes during their entire lifespan, as a Nurse Aide you will be required to work with patients of all ages. Here are some stages of development:
Infancy (birth to 12 months)

Grow and develop quickly
Gain coordination from head to toe
Completely dependent
The toddler Period (1 to 3 years)

Formerly dependent, now gain independence
Develops body control and coordinated movement
Learn to speak, gains bladder and bowel control
The Preschool years (3 to 6 years)

More social interactions
Play cooperatively with other kids
learn language
Know right from wrong
School Age Children ( 6 to 12 years)

Cognitive development (thinking and learning)
Get along with others in peer group
Develop a conscience and self-esteem
Puberty and Adolescence (12 to 18 years)

Secondary sex characteristics appear
Concern for body and peer acceptance
Changing moods due to hormonal changes
Early Adulthood (18 to 40 years)

Select a career, begin experiencing self sustainability
Live with a mate or venture away from childhood home
Raise children and start a family
Middle Adulthood (40 to 65 years)

More comfortable and stable
Has become proficient as a functional member of society
Becomes family foundation
may have “mid-life crisis”
Late Adulthood (65 years and older)

Many physical and psychosocial changes occur
Loss of physical health
Loss of friends and jobs
Begins to think about mortality
Ageism:
prejudice toward, stereotyping of, and/or discrimination agains older persons or the elderly
Remember these facts about aging:
People have many different capabilities
Stereotypes are false
Older persons are usually active
Aging is a normal process, not a disease
They do not need to be dependent
Aging brings many normal changes not considered normal
Thinner, drier, more fragile, and less elastic skin decreases
Weaker muscles
Bones become more brittle
Sensitivity of nerve endings in skin decreases
Short term memory loss
More frequent elimination
Aging brings changes not considered normal
Depression loss of ability to think logically
Poor nutrition
Incontinence
Apathy and Depression

Apathy
A lack of interest.
Major Depression
A type of mental illness that may cause a person to lose interest in everything he once cared about.
Bipolar Disorder
Type of mental illness that causes a person to swing from deep depression to extreme activity.
COMMUNICATION IN SPECIAL SITUATIONS
Patient Anxiety: It is common for patient to be anxious in a doctor’s office, this reaction is commonly known as the white-coat syndrome.
Angry patient: Anger may occur for many reasons. Anger may be a mask for fear about an illness or the outcome of surgery. As a EKG Technician, you will encounter angry patients and will need to help them express their anger constructively.
Patients of other cultures: our beliefs, values, use of language and views of the world are unique to us, but they are also shaped by our cultural background. In any health-care setting, you will most likely have contact with patients of diverse cultures and ethnic groups. Each culture and ethnic groups have their own acceptable behavior, traditions and values. Rather than viewing these differences as a barrier of communication, strive to understand and be tolerant of them.
Patient with visual impairment: when communicating with a Patient who has a visual impairment, be aware of what you say and how you say it. Since people with visual impairments cannot usually rely on nonverbal clues, your tone of voice, fluctuation of speech and volume take on greater importance.

Patient with a hearing impairment: hearing loss can range from mild to severe. How you communicate depends on the degree of impairment and on whether the patient has effective use of a hearing aid. Following are some tips to help you communicate effectively with a hearing-impaired patient:
Find a quiet area to talk and try to minimize background noise.
Position yourself close to and facing the patient.
Speak slowly, so the patient can follow what are you are saying.
Remember that elderly patients lose the ability to hear high-pitched sounds first. Try speaking in lower tones.
Speak in a clear, firm voice, but do not shout, especially if the patient wears a hearing aid.
To verify understanding, ask questions that will encourage the patient to repeat what you said.
Whenever possible, use written materials to reinforce verbal information.
The patient who is mentally or emotional disturbed: when working with this type of patient, you need to determine his/her level of comprehension.
COMMUNICATING WITH FAMILY AND FRIENDS OF PATIENT

Remember that you are representing yourself and the facility to others.
Maintain an open, friendly and supportive relationship with Patients’ families and friends.
Protect Patient privacy and confidentiality as required under the HIPAA Privacy Rule.
When asked, tell family and friends something about the Patient’s activities such as
“He ate a good breakfast” or “She has been very talkative this morning.”
Escort visitors to the supervisor for problems, complaints or reports on a Patient’s condition.
Here are some tips to improve communication:
It is important to remain calm if the patients become agitated or confused.
Avoid raising your voice or appearing impatient.
If you do not understand, ask the patient to repeat what he said.
Terminally patients: terminally ill patients are often under extreme stress and can be a challenge to treat.It is important that health-care professionals respect the right of terminal patients and treat them with dignity
ACCEPTING ONE’S OWN MORTALITY IS A DEVELOPMENTAL STAGE OF LIFE

How to care for dying residents
In a book called On Death and Dying Dr. Elisabeth Ross identified five stages of dying:
Denial: refusal to believe one is dying
Anger: “Why me?”
Bargaining: “Yes, me but…..”
Depression: need to mourn and review one’s life
Acceptance: preparing for death
Advanced directives
Legal documents that allow people to choose what kind of medical care they wish to have if they are unable to make those decisions themselves.
Durable power of attorney for health care
a signed, dated, and witnessed paper that appoints someone else to make the medical decisions for a person in the event he or she becomes unable to do so.
Do-not-resuscitate (DNR)
an order that tells medical professionals not to perform CPR.
All of these factors influence feelings and attitudes about death:
Experience with death
Personality type
Religious beliefs
The following are signs of approaching death:
Blurred vision that gradually fails
diminished sense of touch
decreasing blood pressure
Cheyne-Stokes
Rattling or gurgling sound as person breaths
Incontinence
Cheyne-Stokes respirations
Slow, irregular respirations or rapid, shallow respirations.
Keep these guidelines in mind as you care for dying residents:
Care for mouth and nose
Comfort
Environment
Emotional and spiritual support
Ways to treat dying people and their families with dignity:
Respect their wishes in all ways possible.
Do not isolate or avoid a resident who is dying
Listen if they want to talk
Keep the resident comfortable
Remember hearing is usually the last sense to leave the body
Postmortem Care

